About the KIDNEW project
Chronic Kidney Disease (CKD) knows five stages. Stage 5 is when you will die if you do not receive some form of kidney replacement therapy. Note that presently around 2/3 of the people that worldwide would need kidney replacement therapy do not have access to the therapy because they live in a country that cannot offer it or can only offer it to the very rich part of the population.
From bulky telephones, fax machines, cameras and radios to a smartphone that contains all of these functionalities and fits in your pocket: technological advancements have revolutionized many aspects of our lives in the past fifty years. For kidney failure patients, however, life has remained the same in one major aspect: the dialysis treatment that they rely on for their survival.
It is time for this to change, as the growing prevalence of chronic kidney failure (also known as end stage kidney disease, or ESKD) poses a heavy burden on patients’ lives, and, at €90K per patient per year, also puts considerable financial stress on an already straining European healthcare system.
In short, there is an urgent need for technological innovations to enhance patients’ lives and improve medical outcomes. A very promising route is to enhance the filtration techniques by combining nanotechnology and kidney cells.
Towards better alternatives for dialysis
Dubbed ‘Breakthrough Technologies for an Implantable Artificial Kidney’ (with acronym KIDNEW), this new research project – funded with 3.38 million Euros by the Horizon European Innovation Council (EIC) within the Pathfinder Open 2022 program – brings together EU scientists in the fields of clinical and regenerative nephrology (UMC Utrecht, NL), regenerative pharmacology (University Utrecht, NL), chip processing technology (imec), optical sensing (Optofluid Technologies OÜ, EE), blood compatible coatings (CNRS, FR), and membrane technology (Me-Sep, PL). In the next four years, KIDNEW aims at developing ground-breaking technology that lays the foundation for implantable bioartificial kidneys. This would translate into improved kidney replacement therapy, without the need for immunosuppressive drugs, and at reduced costs.
At the crossroads of chip processing technology and biology
In the body, the kidneys purify blood via passive filtration (by the glomeruli) plus active secretion of toxic waste and active reabsorption of water and useful solutes (by the tubules). In the first step of the KIDNEW project, the team aims to develop advanced nanoporous membranes that allow blood filtration at normal blood pressure (without pumps), just like our natural glomeruli do.
The challenge in fabricating the membrane lies in creating pores that are small enough to not filter out important proteins and spaced together close enough to create a highly porous surface for maximum efficiency. After this filtration step, In the second step, a bioreactor (with specialized kidney cells on a similar advanced membrane) will be used for active secretion of bodily toxins and active reclaiming of useful substances from the filtrate to create urine. The membrane forms the structural backbone for the cells, which will perform their specialized and natural task of regulating the reabsorption of water and important solutes, and additionally the secretion of residual toxins from the blood that cannot be removed by the glomerular filter. Finally, at the end of the project, both pieces will be combined into a prototype bioartificial kidney.
An implantable bioartificial kidney should provide more effective, physiological, and economically sustainable therapy than the current standard of care: dialysis. The eco-friendliness of the proposed technology is in line with the EU Green Deal and highlighted by the European Kidney Health Alliance. The KIDNEW project is configured in such a way that intermediate milestones, planned along the project trajectory, can already be used to support current treatments.
Key objectives of the project
- solid state filter (glomerulus) technology
- solid state active secretion and reclaim (tubule) technology
- solid state integrated biohybrid technology
- technology validation
- contribution to international standards
Project details
Title: Breakthrough technologies for an implantable artificial kidney
Call: EIC Pathfinder Open 2022
Project No: 101099092
Start Date: 01/05/2023
Project Duration: 48 months
Total budget: 3.38M Euro
For additional information please contact the Project Coordinator at the University Medical Center Utrecht or the communication coordinator at imec-NL:
Contact point UMC Utrecht: Dr. Karin Gerritsen, k.g.f.gerritsen@umcutrecht.nl
Contact point for communication and dissemination, imec-NL: Heleen Boers, email: heleen.boers@imec.nl
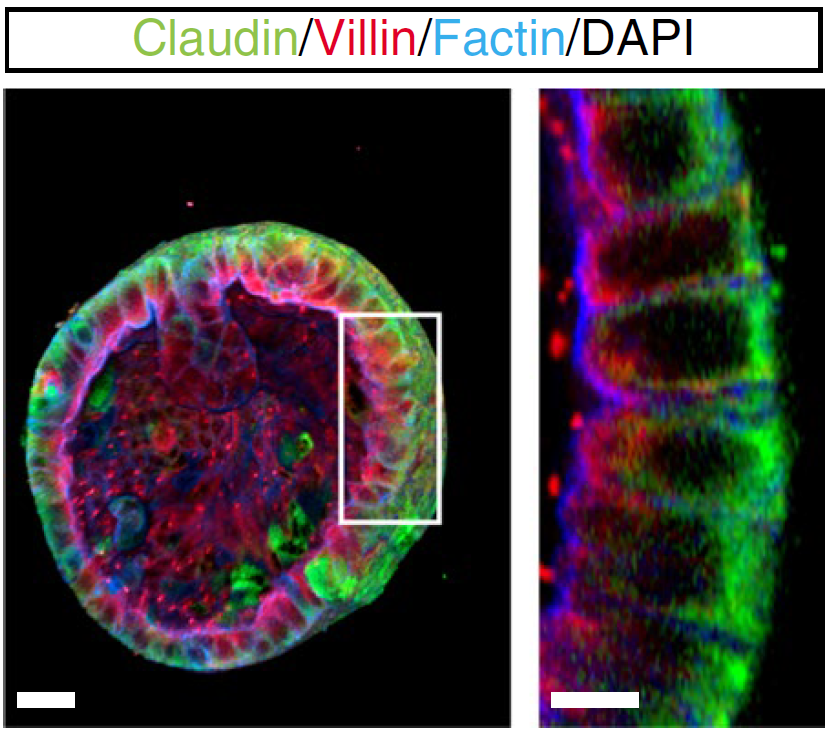
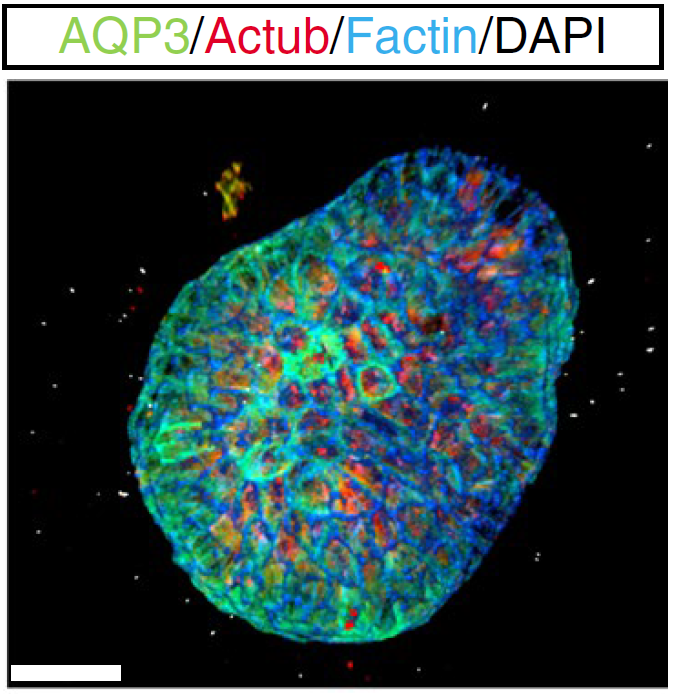
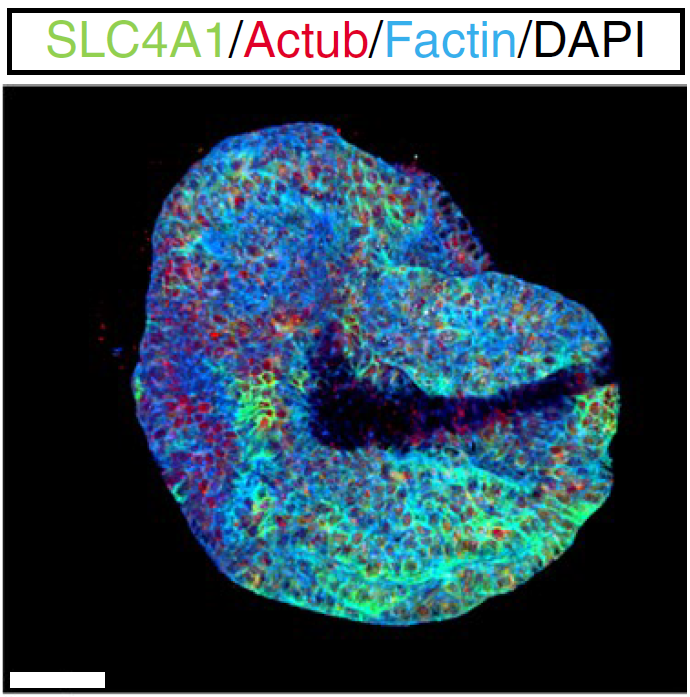
UMCU developed technology to grow adult stem cell (ASC)-derived kidney tubule organoids (tubuloids) from human kidney tissue or urine, shown here with markers of proximul tubule (f) and collecting duct (g, h). ASC-derived kidney tubule epithelial cells from organoids may be used for the tubular exchange unit.
(f) UMCU developed technology to grow adult stem cell (ASC)-derived kidney tubule organoids (tubuloids) from human kidney tissue or urine, shown here with markers of proximul tubule
and collecting duct (g, h)
(h)